8) Pain and Shame
When I first wrote the title of this blog entry, I had in mind a story from a few months ago. But, as it so happens, I just came back this afternoon from seeing the new primary care doctor that my neurologist had asked me to see, and pain and shame ended up being such a huge presence in the room while we were talking that I am instead going to share today's conversation. But first, let me explain why I'm talking about pain and shame and why I'm talking about them together.
Our society has an uncomfortable relationship with pain, and any form of illness which produces it. We're supposed to be tough; in films, in literature, we see people put into a "hero" status if they ignore their pain, grit their teeth and carry on in spite of it. Think about it. How often do we see normal people portrayed as just . . . hurting? How often do you see someone take a bullet, turn to his buddy and say, "Get me to a hospital!" Um . . . never? Even more telling, how often do you see main characters portrayed as the ones in pain, vs. the ones rescuing the people in pain? We all want to be perceived as the strong ones.
Can I just be honest, as someone who lives with physical pain on a regular basis? This is all totally and utterly absurd. Who do we think we're fooling? Who do we think is benefiting from these ridiculous stories we tell each other? There are so many times I want to jump into the TV and just slap the characters around, before shoving in an IV, which they obviously need. But seriously, there is a darker side to all of this, and that's shame. We have an unspoken expectation that people with pain will be dishonest about their pain . . that, just like in books and movies . . they won't really say what they're feeling ("Oh, it's nothing I can't handle") and when they don't live up to this - when they are actually honest about how much pain they're in, it shocks us, and we shame them. This is true of emotional pain as well (which is why depression is still such a huge elephant in our society).
I have talked to friends and acquaintances who have experienced this shaming because of illnesses they have that don't display with physical symptoms that can be seen with the naked eye - such as neurological diseases. Sometimes physicians have difficulty taking patients seriously when the only symptom is . . . pain. Migraines definitely fall into this category. ("It's just a headache, right?") I have often puzzled over the strange irony (at least I find it strange) that modern medicine seems to place such a high priority on saving our life and keeping us alive for longer, but doesn't place nearly as high a priority on improving the years that we have. Why extend the quantity of life if you can't also provide a good quality of life?
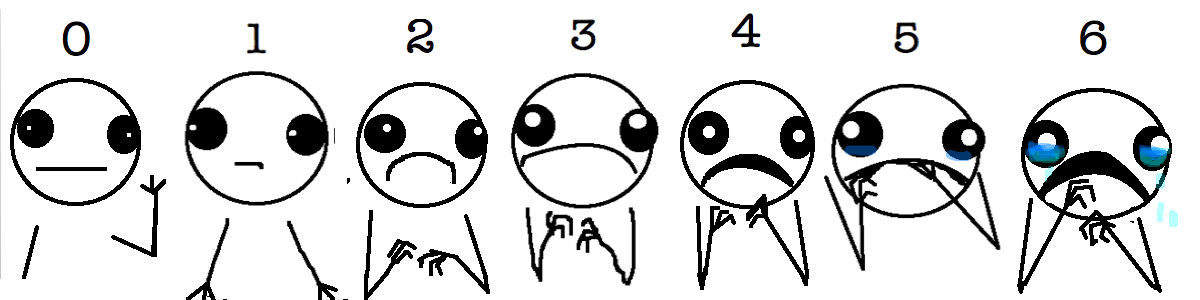
A small but significant example of the way health care providers, perhaps unintentionally, distance themselves from the subject of pain is the completely useless pain chart that they put up on their walls - the 0-10 pain scale, with the faces that barely register any emotional change between "No pain' and "Worst pain I've ever experienced". The thing is, pain IS subjective, and there's no way for one person to crawl into another person's body and experience what they're feeling. Just like so many other things in life, we're relying on communication and trust to establish how we handle it. The thing that irks me about the pain scale - and the whole process of asking patients how they self-rate on it - is that it's not even TRYING to understand what patients are really experiencing. At the very least, that moment could be used to establish some human connection between the person asking (usually a nurse) and the patient, but in all the times I've been asked the question, I don't remember the nurse even looking at me. They're usually looking at their computer so they can type in the response. And do they do anything differently depending on whether you answer "I rate a 5, just your run-of-the-mill pain" or "I'm a 10 - I may be dying"? No. I know this is going to sound harsh, but the way I internalize the experience of being asked the 0-10 question is that they've checked the box by asking me the question, but it's an uncomfortable question to ask so they're not really going to pay attention to my answer.
The best pain scale I've ever seen was drawn by the brilliantly talented and hilarious blogger, Allie Brosh, in her post, A Better Pain Scale. Allie Brosh is most well known for her incredibly insightful writing about depression, which you should absolutely read at some point. But before you read that, read the post about the pain scale because it's really short and will make you laugh out loud but it makes my point much better than I can which is that the clinical environment is totally out of touch with real people in real pain. We'd probably have to make a G-rated version of her pain chart, but I am personally voting for its installation in all hospitals everywhere. See the bottom of this post for a visual of Brosh's pain chart.
All of this is merely context for the conversation I'm about to share with you. Just to recap from a previous blog entry, my neurologist had decided to take me off of a medication that I had been on for my migraines, and recommended that I follow up with a primary care doctor. This was the subsequent appointment with the primary care doctor, someone I was meeting for the first time.
I walked in to the appointment feeling hopeful and positive, in spite of the circumstances. The nurse who took me back from the waiting room and took my vitals was a lovely, warm person dressed head to toe in pink in honor of Cancer Awareness Month. We chatted while she got me settled in the room, and then after a little wait, the doctor (who I'll call "Dr. M") came in.
We shook hands and introduced ourselves, and I briefly explained my reason for being there - how I ended up being on Librium in the first place, how I'd tapered down to 5mg a year ago, how my neurologist, Dr. K, and I had tried to wean me off a few month's ago rather unsuccessfully, and that now I had 2 pills left and Dr. K wanted a primary care doctor to take over this whole situation for her. Dr. M nodded understandingly, and asked me to verify that I was taking Librium for my migraines, rather than anxiety.
"Yes", I repeated, "It was originally prescribed by the Diamond Headache Clinic in Chicago. I was there for a month in 2008, detoxing from a number of medications I had been put on. It's one of several medications I've been taking daily to keep me stable, to keep me out of the hospital."
"I only prescribe this for anxiety. I've never prescribed it for headaches. I also feel unsafe prescribing it for migraines. I mean, this is a benzodiazepine, it's not a safe medicine for you to be on for a long time."
(deep breath from me) "I understand that, and I'm not really happy about it either. I was on 10mg for 8 years, and now I'm down to 5, I tried to get down to 0, but it didn't work. So while I get that this situation is not a good one to be in, I'm in it. I need help figuring out a way forward from here. Would you like to send me to a psychiatrist, since this is an anxiety medicine?"
"Oh no. You're just going to have to make do with the 2 tablets you have. Maybe you can break them in half, so you're taking a 2.5 mg dose for a few days."
"Um, ok. How does that work? They're capsules. You can't really cut them in half."
"Just use the powder inside the capsule." [A mental image of me doing a line of Librium floats through my head.]
"Ok, I'm not sure I understand that, but even if I can get the powder, we already know because I've tried to do this in the past, that my body has a tough time coming off of this pill, and that's with more time and more pills than you're giving me here. So I can pretty much expect that the side effect is I won't be able to sleep, which triggers my migraines, which may mean I end up in the ER. Are we ok with that outcome?"
"You've just got to tough it out. This is not a good medicine for you to be on, and you've got to come off of it sometime. I can't prescribe this for migraines. You are taking this for migraines, right? Because I only prescribe this for anxiety.
Pause. At this point in the conversation two things are happening on my end. First, I am really and truly panicking. In all of the hundreds of places I have received care, all over this country, outpatient, inpatient, from countless physicians, I have never encountered one who did not consider it important to try and avoid my pain and suffering. All of them factored this in to their decision-making. But Dr. M did not seem terribly concerned about it. Second, it seemed odd to me that she kept asking me what I was taking the medicine for since I had clearly explained that it was the Diamond Headache Clinic that had prescribed the medicine. The thing is, I do have a depression/anxiety diagnosis on my charts - it's something that I take two additional medicines for (Dr. M mentioned this very thing when she first walked in the room), so I could have told her - "Oh, it helps me with my anxiety too", but this seemed dreadfully dishonest because it wouldn't have been true. This was one of those situations where the very system built to help protect patients was hurting me. Dr. M was concerned about why I was taking it because of what she needed to log in her charts, and what she logged in her charts was because of protocols that are meant to protect patients. But what you need to truly protect patients is trust between the patient and provider, so that communication breakdowns like the one that she and I had do not occur. If Dr. M were a small town physician who knew me, she wouldn't have cared that I wasn't taking Librium for anxiety because what matters is what to do going forward. She was asking the wrong question. What I needed from her was to ask me an open-ended question, such as:
"Tell me about your experience trying to come off this medicine a few month's ago. What happened?"
If she had been able to just sit and listen for a couple of minutes and hear about my pain and anxiety, perhaps the whole outcome of the conversation would have been different.
When I expressed my fear about what could happen, this is how the conversation went.
"Dr. M, I'm getting scared here. Lack of sleep is a major trigger for me. It's very consistent. If I don't get enough sleep, I can guarantee I'll get a migraine."
"Yeah, well, don't we all."
There are so many things I wish I had had the presence of mind to say in response to this callous, flippant statement, but in the moment I just stumbled out with,
"You get migraines too? Have you had to go to the ER with them?"
"No, but that's because I know how to control them."
Let's just pause here and analyze what's going on in this room. Dr. M is clearly feeling fear - I'm not sure exactly why, but I can make an educated guess based on what she has told me. She's told me that she doesn't want to prescribe Librium for migraines; she only prescribes it for anxiety. She doesn't like that I've been on the drug for a long period of time. Ok, so, Dr. M has no experience prescribing this drug for my condition, and doesn't want to be responsible for doing so. She's clearly constricted by Kaiser's strict protocols and doesn't want to get flagged for doing something that is outside of those protocols. Again, I'm making an educated guess. But the fact that she can't admit her fear to me, and that I'm putting pressure on her causes her anxiety to spike, and the result is that she probably does something out of character which she later regrets - she shames me. And this shaming, associated with pain and my need to alleviate it, is something that I encounter all too frequently in the healthcare system. Which means that I am now triggered, and angry, on top of everything else, which causes our communication to completely break down and any fragment of trust we might have had to disappear. This is evidenced by one of the last parts of our conversation.
(Me) "So I'm trying to think of solutions for the insomnia, since that will be the main challenge. Would you be willing to give me a small dose of Ambien to get me through the rough patch?" (background: I had Ambien prescribed for insomnia by another primary care doctor at Kaiser, and it didn't seem to be a problem)
(Dr. M) "Oh, so this is turning into a negotiation? No, I don't think so. I'm going to give you an antihistamine, which should help you sleep." (antihistamines never help me sleep, but then - she didn't bother to ask me about that)
"Don't you support the idea of shared decision-making? I'm just trying to figure out a way through this."
"That's not what this is about."
And with that, Dr. M walked out of the room.
*For the record, I did attempt to engage Kaiser's management by speaking to Member Services after this conversation. My formal request (to reconsider the decision about the medicine) was denied. I also sent them this entire blog entry, to which they never responded. And as I had predicted, I did end up in the ER 3 weeks after this appointment.
Credit goes to http://hyperboleandahalf.blogspot.com/2010/02/boyfriend-doesnt-have-ebola-probably.html - A Better Pain Scale